Abstract
Background
Allogeneic stem cell transplantation (allo-SCT) using an HLA-matched sibling donor remains the only curative treatment for young patients with acquired severe aplastic anemia (SAA) [1]. When a matched sibling is not available and a patient does not achieve a response to immunosuppressive therapy (IST), allo-SCT from an unrelated donor (URD-SCT) is the preferred alternative. However, haplo-SCTs are increasing as a graft from a related mismatched donor is readily available for most patients and has the advantage of allowing for prompt transplantation. Therefore, haplo-SCT is a front-line therapy option for very SAA (VSAA) when the patient is not able to receive a SCT from emergent compatible donors.
Methods
We collected clinical data on 38 consecutive patients with aplastic anemia (AA) all of whom were treated at the Lu Daopei Hospital between December 2013 and July 2020. Patients had a median age of 8 (range: 1-34 years), 21 patients were male and 17 were female. Of the enrolled patients, 4 had 4 congenital AA, 34 had acquired AA and 3 had hepatitis-associated SAA. Median time from diagnosis to transplant was 9 months (range: 1-282 months). Eleven (28.9%) patients failed to receive ATG/ALG treatment. Twenty-six patients received a haploid-SCT, three patients received a sibling HLA-matched SCT and 9 patients received a URD-SCT. The sources of donor stem cell were parents in 11 cases, brothers and sisters in 6 cases, and unrelated donors in 9 cases. Median age of the donors was 32 (range: 11-57 years). Moreover, there was 13 donors that were incompatible in blood type with the patients. With regard to HLA matching type, 16 patients were HLA 5/10 and 22 patients were ≥ HLA 6/10. The stem cells were derived from BM+PBSC in 29 cases and from PBSC in 9 cases. The median dosage of MNC transfusion was 12.385x108/kg (range: 4.97-29.44x108/kg), CD34+ cell transfusion was 9.42x106/kg (range: 2.64-22.4 x106/kg) and CD3+ cell transfusion was 2.26 x106/kg (range: 1.11-7.92 x106/kg). Preparative regimen were Flu/Cy/ATG+TBI 200cGy for 30 patients, Bu for eight of the patients and three patients received BU+TBI. Additionally, all patients were treated with CSA/FK506 + MMF + sMTX to prevent GVHD.
Results
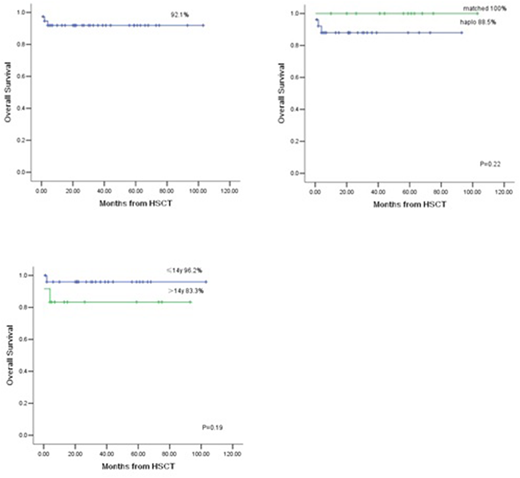
The median follow-up was 26.5 months (range: 1-103 months). All 36 cases were engrafted and no primary graft failure occurred. There was only one case of secondary graft failure. The median day of leukocyte engraftment was day +13 (range: +10 to +23), the median day of platelet engraftment was day +10.5 (range: 6-167). An Evaluation of bone marrow at one month after transplantation showed all patients were fully donor type. The overall survival (OS) rate was 92.1%, OS for haplo-SCT was 88.5%, and OS for HLA-identical SCT (sibling HLA-matched SCT + URD-SCT) was 100% (Figure 1).
Conclusions
In conclusion, the outcomes of haplo-SCT with TBI 200 cGy/Flu/Cy/ATG indicate that haplo-SCT can be an effective alternative option for SAA patients when fully matched or unrelated matched donors are not available, or for patients with VSAA who need an urgent transplant.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal